Hastings Prototypes
 | Medicalising Poverty: Helping Primary Care Refer People to Fuel Poverty The aim of this prototype is to help GPs identify patients who are at risk of respiratory illnesses due to living in cold houses, and texting them about available services, such as home checking, support with cold homes, energy advice etc. | 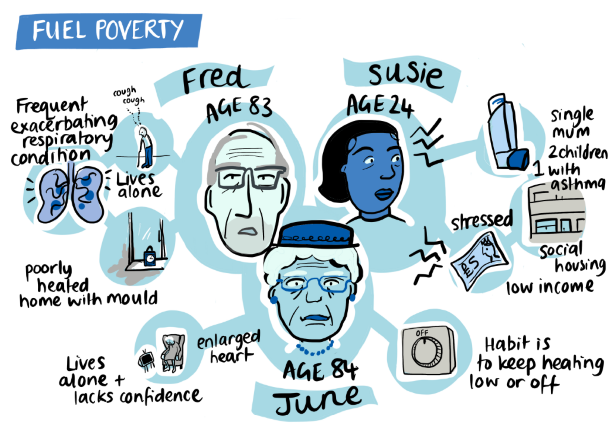 |
 | Medicalising Poverty: Wider uptake and further provision of sports and activities to support healthy living (focusing on children and young people) |  |
 | Medicalising Poverty/Rationing: Designing a pro-active GP appointment system for long-term high intensity users This prototype is using an evidence-based approach to focus on long-term high intensity users who will be also attending the practice frequently in the future unless changes are made. There are many different segments within this, by age and health condition, but an initial target selected for focus is young women with complex family and life backgrounds. One practice is leading as a pilot, where a number of different approaches are being implemented – GP continuity for appointments and linking to a Health & Well Being coach and programme. The same analysis has been run across all practices in the PCN to show all practices that they have similar cohorts of long-term high attending patients. | 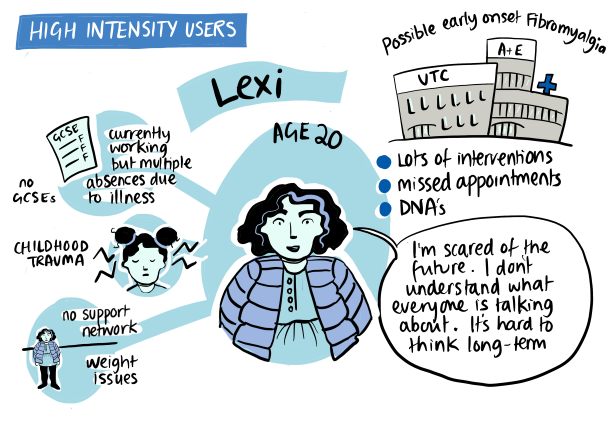 |
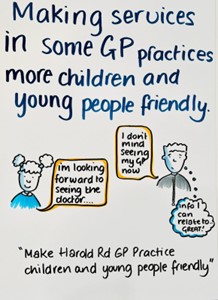 | Rationing: Developing children and young people friendly practices This prototype group are focussed on making services in some GP practices more accessible for children and young people. We plan to do this by upskilling trained community assets that already exist to advocate for young people by a trusted triage system. The voluntary sector will be the first port of call, children and young people will be referred to GPs from there. | 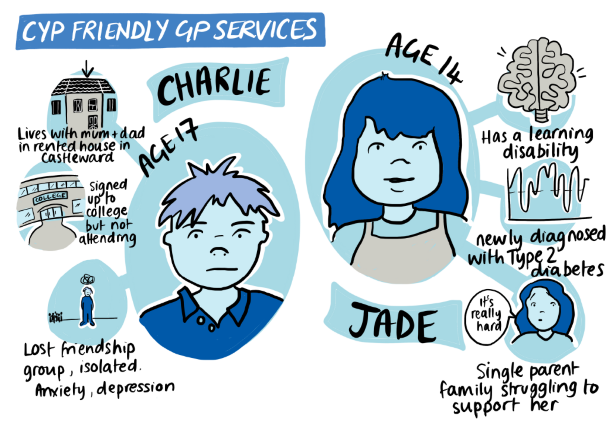 |
 | Access: Testing the Ability to provide ‘no wrong door’ access to service users. Do services users understand why organisations want to share data, and its benefits? This prototype group would like to establish a method of data collection through which data is shared across organisations. The idea is that the patient would be able to go to any service because their data would be shared across organisations | 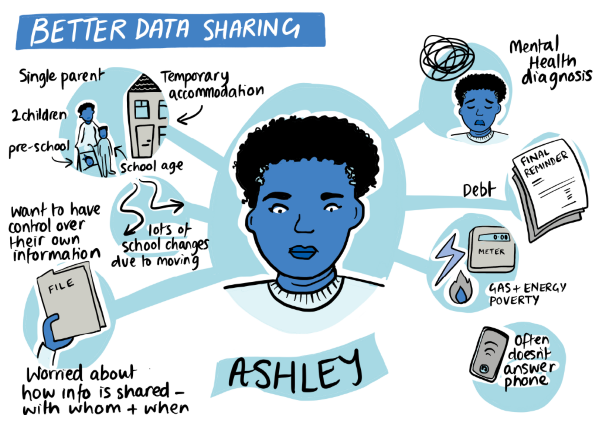 |
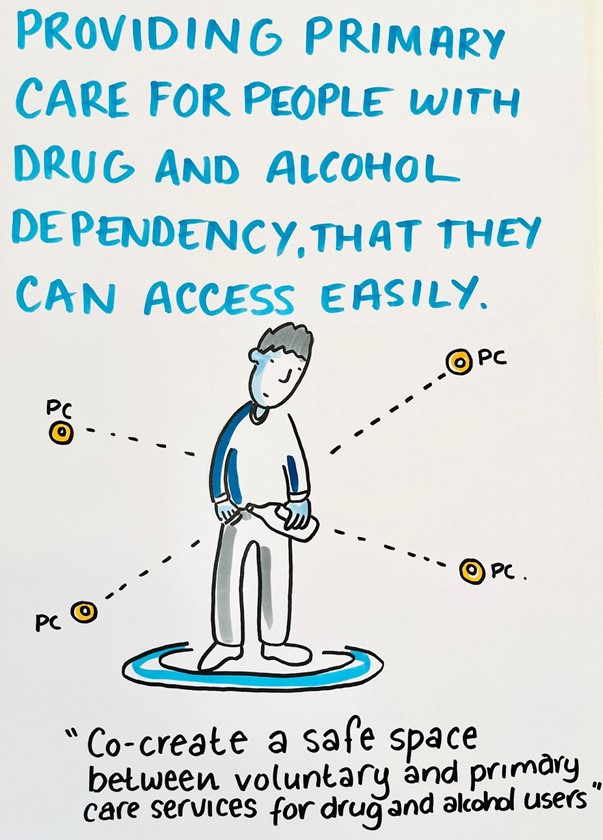 | Access: Designing a needs-based model of primary care for people with drug and alcohol dependency (in the community) This prototype’s plan is to help people with drug and alcohol dependencies to get back in the healthcare system in a supported way. How do we bring the health support into a place where they feel safe? | 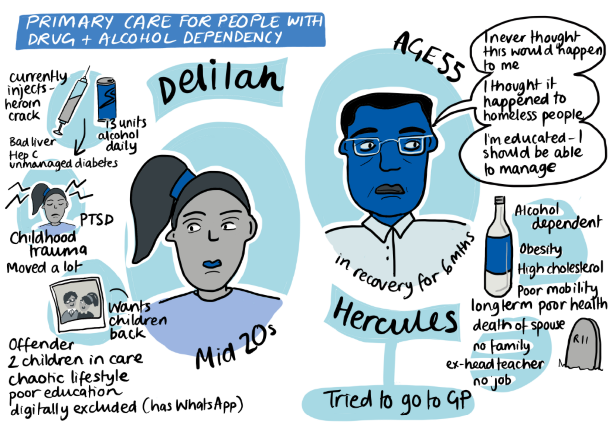 |
 | Access: A ‘Health Fair’/ pop up hub in the precinct to showcase the services available to people This prototype centres around establishing a ‘health fair’, which will focus on offering help and access to service users. The next step is working on how to spread from the Health Fair into practices, taking the information from the Health Fair and helping practices understand what’s available. | 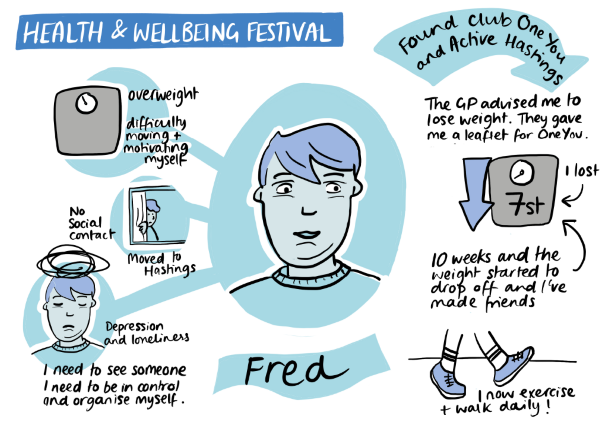 |
 | Access: Accessing Translation Services in Primary Care This prototype seeks to improve translation services in Primary Care and use them in a focused way. The challenge is where non-English speakers cannot navigate GP access systems to describe their needs or get an appointment. Currently translators have to act more as carers than translators and spend long periods of time on hold trying to get an appointment. Also, they often inappropriately hold personal and confidential information about these patients. This prototype group would like to create a more streamlined service to be able to contact general practice. We are seeking to test out our prototype in a handful of GP practices. | 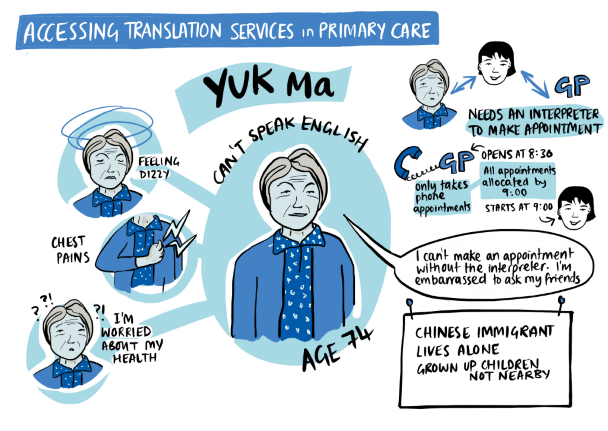 |
 | Access: Open Access English for all This prototype begins from the perspective that all residents should be empowered to have ownership of their access (to healthcare and other services, including employment/education) by offering opportunities to improve their English. We want to move people from being reliant on translation services to learning English themselves, using a community led model designed in a ‘pay it forward’ style. This is a widely co-produced service across the UH workshops and an active Whats App group that has managed to identify a location, a time and a lead teacher, and a number of different areas of learning. English courses are being offered twice a week and a series of additional learning workshops are planned - e.g., IT skills, e.g., GP trainees coming in to run simulated appointments. | 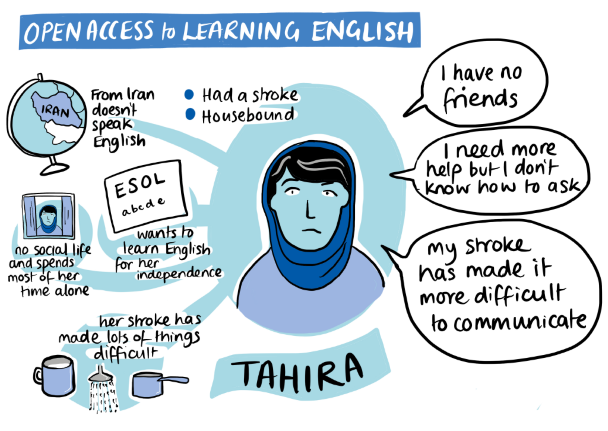 |
 | Access: Ensuring prescriptions can be delivered promptly | 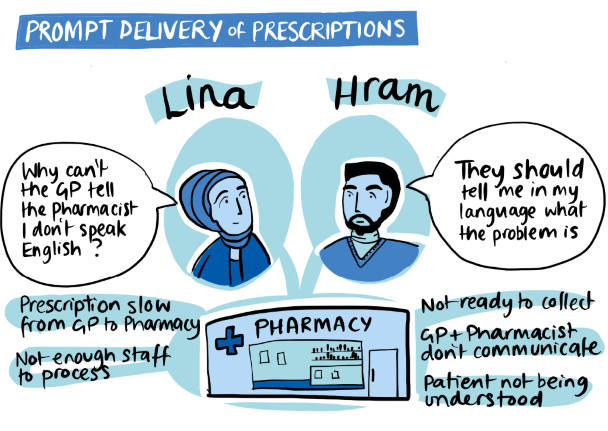 |
 | Recruiting the Clinical Workforce Locally: Creating a path into healthcare work for local people It is important for children and young people to be exposed to the opportunities and available careers in medical sciences to support and inspire future generations. This prototype group are working towards making careers in medical sciences accessible and exciting to children and young people. |  |
How the NHS can support the Voluntary Sector to improve health This programme of work has been to make the most of the learning and experience across the two partner ICSs, in developing ways the NHS can enable the Voluntary Sector to be a valuable partner and to help meet need and reduce demand through early intervention and community based support. Here we are collaborating on designing the model. |